Case Report: Primary Hyperparathyroidism, (masquerading as) Hyperemesis Gravidarum and Parathyroidectomy[1] in Pregnancy[2]
Author (Corresponding): author@hgandphpt.com
Disclaimer: The author is not a medical professional or student, and is presenting this case report as a family member of the patient, information is taken from memory and records the author had access to. This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector. This essay was not peer-reviewed and is not suggested to be used for academic or medical purposes.
A story of this case report has been published on hyperemesis.org, click this link to read. |
Click here for a collection of 40+ related Articles and Case reports |
Primary hyperparathyroidism is one of the most common endocrine disorders in the general population but is rarely diagnosed during pregnancy and its presentation ranges from non-specific symptoms to hypercalcemia. Hyperemesis gravidarum has been shown to be significantly increased in pregnant women with primary hyperparathyroidism. A 27-year-old patient, 10 weeks pregnant, presented to the emergency department with a 3-4-week history of nausea and vomiting. She was initially diagnosed with hyperemesis gravidarum. Her symptoms persisted until hypercalcemia was discovered. Her workup led to a diagnosis of primary hyperparathyroidism caused by a LR parathyroid adenoma. The patient was hospitalized for a period of 37 days during which she was treated with aggressive intravenous hydration, electrolyte replenishment and chemical balancing, two abnormal parathyroid glands were found, and successfully removed in the 2nd trimester, which led to complete resolution of the symptoms within a matter of days.
KEYWORDS: endocrinology; pregnancy; hyperemesis gravidarum; primary hyperparathyroidism; parathyroidectomy; hypercalcemia; hypokalemia; hypomagnesemia; maternal and obstetric complications.
Endocrine disorders in pregnancy are challenging as regards diagnosis and treatment. Primary hyperparathyroidism (PHPT) is the third most common endocrine disorder, often asymptomatic. The author reports the management of a symptomatic case during pregnancy.
In October 2019 (Oct 29) A 27-year-old patient, G4P3A0, with a 10-week pregnancy, consults for 4-week-old nausea and vomiting, accompanied by weight loss (approximately 10lbs or 6.57% of pre-pregnancy weight) and fatigue was diagnosed as hyperemesis gravidarum (HG). The patient denied any major medical history, myalgias, abdominal or flank pain, dysuria, chest pain dyspnea, cough, sputum but confirmed the presence of severe nausea and vomiting during prior pregnancies.
At the first exam, done in a clinical setting at 8 weeks pregnant the outcomes were: sodium (140 mmol/L), potassium (3.1 mmol/L), creatinine (45 umol/L). The patient was treated with 2L Normal Saline (NaCl 0,9%) daily (q12h) and 50mg Dimenhydrinate (antiemetic) BD (twice daily) in a home care setting.
During her routine pre-pregnancy (10 weeks) visit the OBGYN supported the prior diagnosis of HG but ordered more testing which revealed hypokalemia (2.9 mmol/L) and hypomagnesemia (0.57 mmol/L), creatinine (42 umol/L), in addition calcium total (2.96 mmol/L) didn’t cause alarm (yet).
The patient was instructed to present to the Emergency Department (6 days after original exam) during which the exams were repeated and confirmed potassium (2.9 mmol/L). Patient was treated with 20 mmol K PO and instructed to return for re-verification of potassium levels. (It is unknown to the author why there was no testing done for magnesium and calcium levels as they were both outside of normal range on prior tests).
Patient returned to the ER 5 days later as instructed to re-verify her potassium (2.9 mmol/L); Mg (0.61 mmol/L) workup also revealed Ionized Ca (1.66 mmol/L) (reference range 1.1–1.3 mmol/L). The Internal medicine team was consulted, and suspected the hypercalcemia was secondary to primary hyperparathyroidism and worsened by the vomiting. The patient had no family history of hypercalcemia.
Subsequent workup showed PTH at 21.8 (reference range 1.50-9.30)
A neck ultrasound completed 2 days after admission noted hypoechoic nodules measuring 9 x 11 x 12.4 cm related to the inferior pole of the right thyroid lobe concerning for right parathyroid adenoma. Given the high risk of spontaneous abortion, preterm labour, and underdevelopment of the parathyroid glands in the fetus, the patient was evaluated by an Endocrine surgeon who recommended parathyroidectomy and four-gland exploration in the second trimester.
Normal sonographic appearance of both thyroid glands the right lobe measures 1.4 x 1.9 x 4 .3 on, a left lobe
measures 12 x 12 x 4.3 cm. No nodules are abnormal vascularity. No size significant cervical lymph nodes.
During her admission (37 Days), the patient's hypercalcemia and concomitant electrolyte abnormalities (hypokalemia and hypomagnesemia) were managed medically by Obstetric Medicine and Endocrinology. Patient was mainly treated with high rate IV Fluids (Furosemide was recommended patient advocated for strict I/O instead and was able to maintain acceptable ratio), calcitonin (PRN if Ca ≥2.9 to avoid tachyphylaxis, Drs. recommended against cinacalcet as being unsafe in pregnancy), and antiemetics. The (presumed) hyperemesis gravidarum was managed by OBGYN and Nutrition. She had a dramatic initial response to antiemetic treatment with partial resolution of her symptoms and improved PO intake; however, after that patient had ongoing nausea and vomiting with minimal PO intake and persistent weight loss throughout her hospitalization.
IV access was lost quite often but patient declined picc line and provided reason to avoid risk of infection and thrombosis, on occasion anesthesia was needed for insertion. Mostly the patient had two peripheral IV lines to support the fluid volume, Chem 7 profiles were taken daily.
32 days after admission the endocrine surgeon performed a four-gland exploration with RL and LL parathyroidectomies. There were no complications of anesthesia or surgery. Following the surgery, the patient reported having diffuse muscle aches. The patient was treated medically by Endocrinology for hypercalcemia. The muscle aches and laboratory abnormalities resolved, and the patient was cleared for discharge by endocrinology and general surgery. Upon discharge, the patient is feeling well. (Has lost 20lbs from her pre-pregnancy weight or 13.15%) She will be followed as an outpatient with (Endocrinology) and (Surgery).
In May 2020 at 39w4d the patient gave birth to a full-term healthy Baby boy weighing 3160g and measured 55.5cm.
Habits:
Medications during hospitalization:
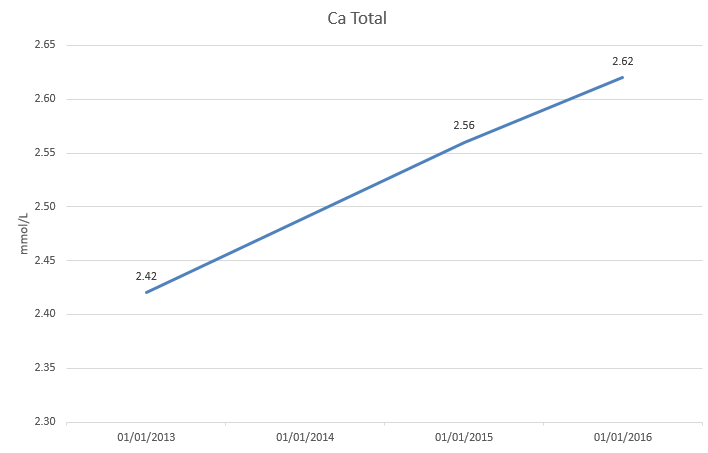
The patient had a history of calcium on the higher end of normal range, the author had access to several tests done prior to this ordeal which gives us an idea of the uptrend in Ca levels:
Reference range 8.5-10.5 (4.3 to 5.3 mEq/L or 2.2 to 2.7 mmol/L)[4]
Figure 1 Serial calcium levels prior to diagnoses
Is there a chance the severe nausea and vomiting the patient experienced during prior pregnancies was a result of elevated Ca?
Since Hyperemesis gravidarum (HG) is a diagnosis of exclusion we can only attempt to properly diagnose during future pregnancies.
Outcome of PTH:
Figure 2: PTH Levels from diagnosis to post op
[1] Seventeen Cases of Primary Hyperparathyroidism in Pregnancy: A Call for Management Guidelines https://academic.oup.com/jes/article/3/5/1009/5342947
[2] Primary Hyperparathyroidism Mimicking Hyperemesis Gravidarum https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3555476/